7th SA TB Conference 2022 Poster Presentation
Track 3: Implementation/Health systems
Authors: Marcel Kitenge1,2, Ruvimbo Chingonzoh3,4, Abraham L.Malaza1, Mcedisi J. Madlavu3, Riyadh Manesen1
1THINK TB & HIV Investigative Network, Hillcrest, KwaZulu- Natal, South Africa. 2Division of Epidemiology and Biostatistics, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa. 3Division of Public Health Surveillance and Response, National Institute for Communicable Disease, National Laboratory Services, Johannesburg, South Africa. 4HIV and AIDS, STIs and TB (HAST) Programme, Eastern Cape Department of Health, King Williams Town, South Africa.
Background
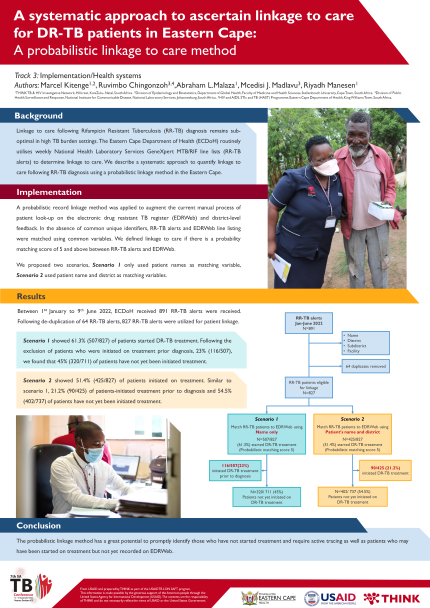
Linkage to care following Rifampicin Resistant Tuberculosis (RR-TB) diagnosis remains sub-optimal in high TB burden settings. The Eastern Cape Department of Health (ECDoH) routinely utilises weekly National Health Laboratory Services GeneXpert MTB/RIF line lists (RR-TB alerts) to determine linkage to care. We describe a systematic approach to quantify linkage to care following RR-TB diagnosis using a probabilistic linkage method in the Eastern Cape.
Implementation
A probabilistic record linkage method was applied to augment the current manual process of patient look-up on the electronic drug resistant TB register (EDRWeb) and district-level feedback. In the absence of common unique identifiers, RR-TB alerts and EDRWeb line listing were matched using common variables. We defined linkage to care if there is a probability matching score of 5 and above between RR-TB alerts and EDRWeb.
We proposed two scenarios, Scenario 1 only used patient names as matching variable, Scenario 2 used patient name and district as matching variables.
Results
Between 1st January to 9th June 2022, ECDoH received 891 RR-TB alerts were received. Following de-duplication of 64 RR-TB alerts, 827 RR-TB alerts were utilized for patient linkage.
Scenario 1 showed 61.3% (507/827) of patients started DR-TB treatment. Following the exclusion of patients who were initiated on treatment prior diagnosis, 23% (116/507),
we found that 45% (320/711) of patients have not yet been initiated treatment.
Scenario 2 showed 51.4% (425/827) of patients initiated on treatment. Similar to scenario 1, 21.2% (90/425) of patients-initiated treatment prior to diagnosis and 54.5% (402/737) of patients have not yet been initiated treatment.
Conclusion
The probabilistic linkage method has a great potential to promptly identify those who have not started treatment and require active tracing as well as patients who may have been started on treatment but not yet recorded on EDRWeb.